10/17/2016

Problems with the patella are among the most common causes of knee pain. The pain is typically “anterior”, or in the front of the knee, or in, behind, or around the patella. Patella pain may be associated with other symptoms, such as instability or giveaway, dislocation, catching, grinding (crepitation), and/or swelling. Any or all of these symptoms may present spontaneously, or following injury, such as with a direct blow to the front of the knee, or after a dislocation or partial or temporary dislocation, called a subluxation.
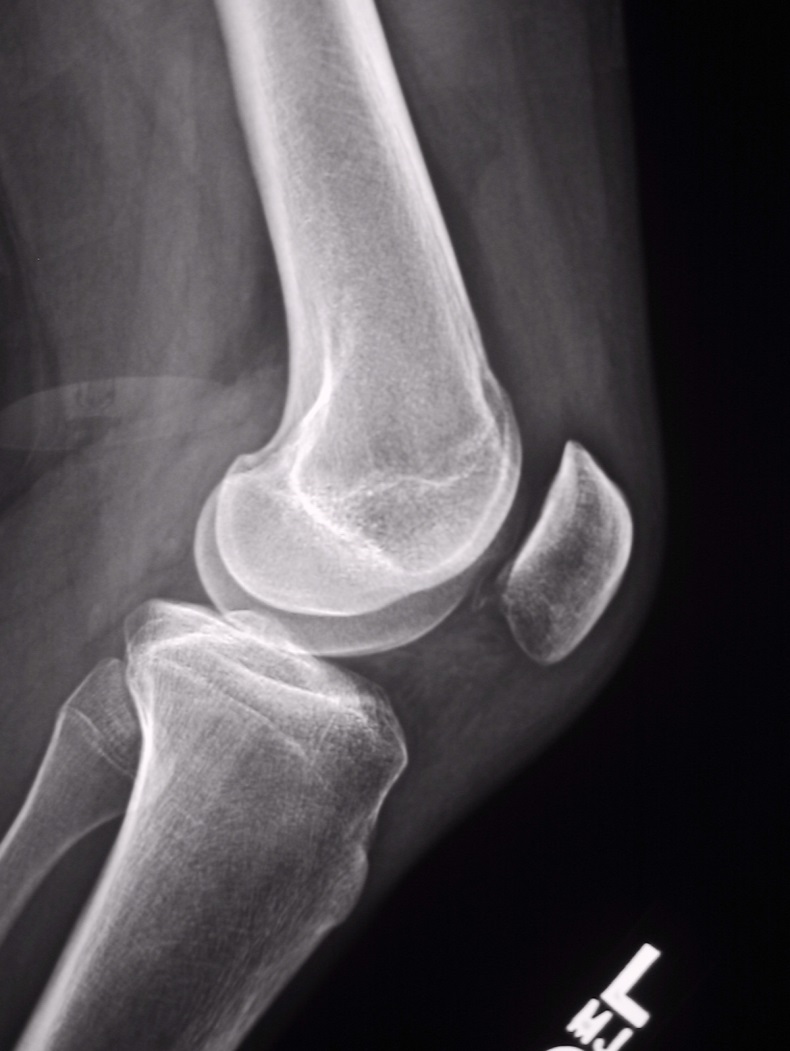
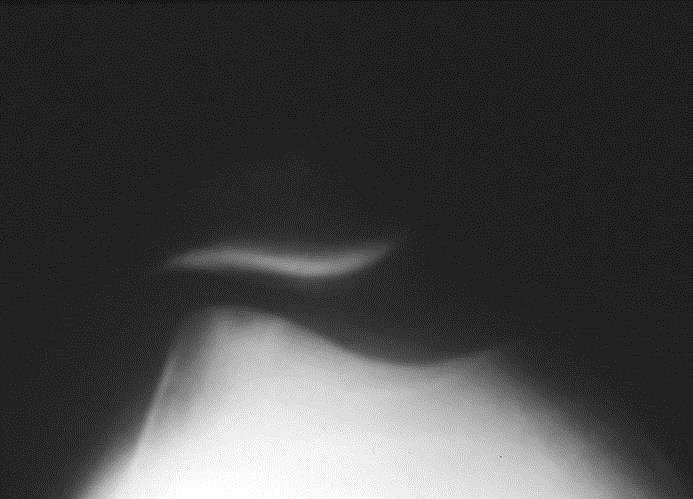
Here are two X-rays that illustrate the best views of the patella. The top view is called a “Merchant’s view” and is obtained with the knee bent 45-degrees, with the beam of the X-ray photograph directed through the knee from head to toe. It shows how well the patella is aligned within the groove on the femur, called the trochlear groove. The bottom view is a lateral view, and is obtained from the side of the knee. It shows the height of the patella relative to the knee joint. A high-riding patella is called patella alta, and can be associated with instability of the patella, as it is not well-engaged in the trochlear sulcus with the knee near full extension (knee straight). A low-riding patella is called patella baja.

Here is an axial MRI view of the patella within the trochlear groove of the femur as seen with the knee in full extension (straight). Here we also get an indication of the alignment of the patella, and we can also get a sense of how healthy the cartilage is on the back of the patella. Normally, the hyaline cartilage on the back surface of the patella is thicker than anywhere else in the body. Problems with the cartilage on the back of the patella include softening, blistering, fissuring, erosion, and thinning. These problems are collectively called chondromalacia patella. It is important to note that MRI assessment of patella cartilage is not always accurate. CT scanning also may be useful to assess patella alignment.
CLASSIFICATION OF PATELLA PROBLEMS
Patella problems can be organized in a number of ways. For instance:
1- Pain alone: “patellofemoral syndrome”,
2- Pain from malalignment, i.e.- tilt and/or displacement,
3- Instability: subluxation and dislocation,
4- “Wear and tear”, i.e.- chondromalacia patella or arthritis,
5- Other problems from pain around the patella: e.g.- synovial plica, tendonitis, bursitis, Osgood Schlatter’s disease, etc.
MANAGEMENT OF PATELLA PROBLEMS:
The vast majority of these patella problems respond well to non-operative, conservative treatment, which may include: special exercises (physical therapy, home exercise programs, closed chain strengthening, etc.) to strengthen the quadriceps and hip muscles or improve the flexibility of the hamstrings and IT band, knee sleeves or braces, patella taping, foot-arch supports (orthotics), medications (Tylenol or NSAID’s), icing, and weight loss.
Relative rest from aggravating activities like running, jumping, or aggressive weightlifting, may be helpful. Knee sleeve braces or taping help with quadriceps muscle function for patella alignment. Exercises that are especially useful include cycling, leg press, rowing, swimming and treadmill or outdoor walking. It is wise to avoid “open chain” knee exercises, like the knee extension machine. Small amounts of weight loss can make a huge difference with patella pain, e.g.- ten pounds of weight loss reduces patella loads by 60-120 pounds at the knee for daily activities such as squatting and stair climbing.
Surgery is rarely necessary, and must be carefully considered, as it may make the problem worse in poorly selected cases, and sometimes even in well-selected cases. It is best used as a last resort, after all else fails. Surgery will vary depending upon the type of patella problem. It is most often indicated for cases of malalignment and instability, and not a good choice for pain without malalignment or instability. Arthroscopy is the very best way to evaluate the patella and surrounding portions of the knee joint.
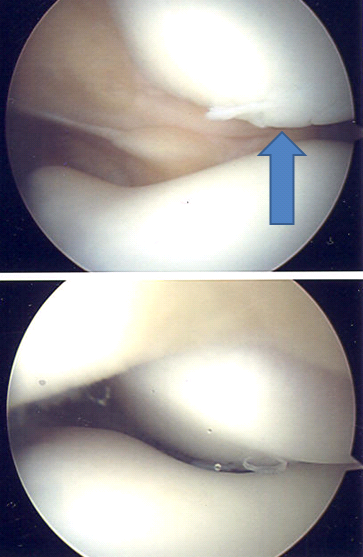
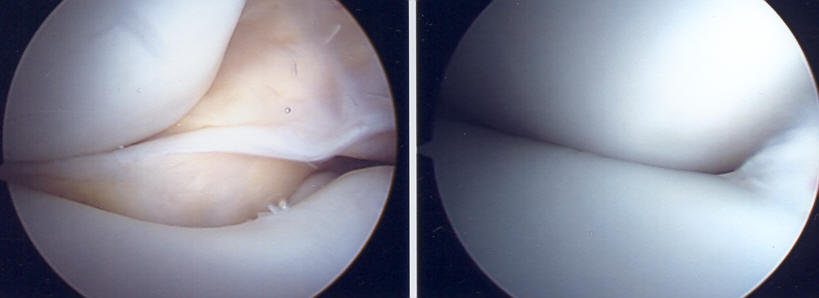
A typical arthroscopic top-to-bottom (“head-to-toes”) view of a malaligned, laterally displaced right patella in full extension (top), and with improved tracking as the knee flexed beyond 45 degrees (bottom). Note the rough surface of the patella, blue arrow. This is known as “chondromalacia patella”, and is a common finding, even in knees without patella pain.
Here is a view of more advanced chondromalacia, affecting BOTH the patella (yellow arrow) and the trochlear groove; note the fissuring and fibrillation, i.e.- roughness of the surfaces:
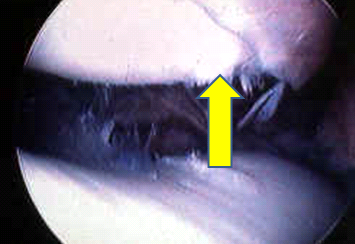
This roughness can cause grinding (crepitation), pain, catching, and giveaway symptoms, and can cause swelling.
Here are some arthroscopic views of a “synovial plica”:

Arthroscopic view of a left knee pathologic “synovial plica” (top), a band of tissue like a shelf which can become trapped between the patella and the femoral sulcus, and cause medial pain or periodic catching or snapping sensations at the medial side of the patella. These can be easily removed or resected (bottom).
SURGERY FOR PATELLA INSTABILITY AND MALALIGNMENT:
Although surgery is usually a last resort, occasionally it may be an option for those who fail a reasonable trial of conservative care, as outlined above. It is BEST performed for patellas that do not line up properly within the femoral trochlear groove, and/or for patellas that subluxate or dislocate, i.e.- “pop out” of the groove. Surgery is rarely, if ever, indicated for patella pain alone, and it may even make pain worse.
Malalignment is typically the result of three basic factors:
1- tightness of the lateral tissues (lateral retinaculum),
2- looseness of the medial tissues (medial patellofemoral ligament and retinaculum),
3- excessive “Q-angle”, i.e.- a patella tendon that inserts too far laterally on the tibia below the patella (on the tibial tuberosity).
Any or all of these factors may contribute to the problem, and therefore, different surgical choices for correction exist, which will be influenced by the surgeon’s experience and judgement, and the patient’s risk tolerance.
Here are examples of Merchant’s X-ray views of various types of patella malalignment:
Mild tilt alone…

Tilt combined with displacement…
Tilt and displacement and arthritis…

These three patients, having failed conservative care, would represent completely different surgical options, although all three may present with similar complaints.
Surgical options include:
1- lateral release, to loosen the tight lateral structures,
2- medial repair and reconstruction, or tightening of deficient medial tissues,
3- tibial tuberosity bone medial transfer procedures to correct the abnormal insertion of the patella tendon on the bone, and hence, correct the Q-angle.
The first two can be done with arthroscopic means and small incisions or portals, but the latter requires an open approach, cutting the tibia bone with a small saw, and moving the tibial tuberosity, and screwing it down in a better location, to move the patella into the groove.
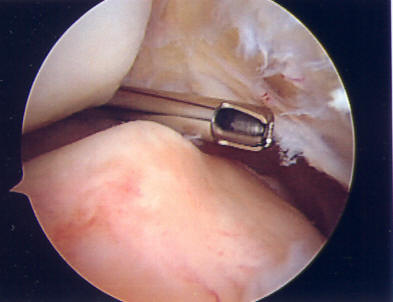
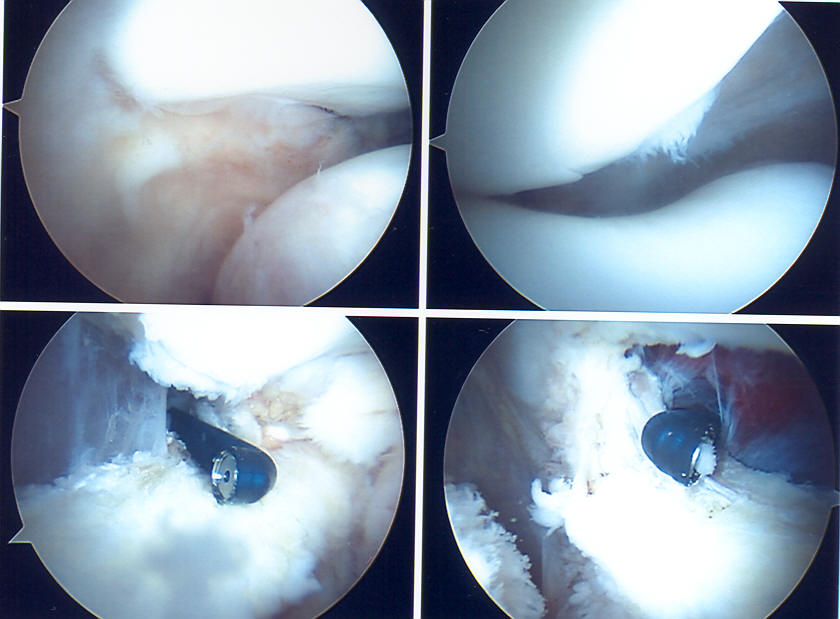
A lateral release is an arthroscopic procedure done to correct a tight lateral retinaculum, and involves cutting these tissues. It is only done for malalignment alone without significant instability. A specific condition called LPCS (lateral patella compression syndrome), or ELPS (excessive lateral pressure syndrome) with negative lateral tilt of the patella may be improved with a lateral release and aggressive post-operative rehabilitation. Below are four arthroscopic views of the patella from top-down (head to toes view), which show malalignment, and cautery of the margins of the release to reduce post-operative bleeding. This procedure can be done under LOCAL ANAESTHESIA.
More significant malalignment or frank instability usually requires more extensive surgery with bigger incisions to improve alignment and reduce or correct symptoms. These include tightening of the medial tissues which serve as a “check-reign” to the lateral motion of the patella, or transfer of the attachment of the patella tendon to realign the patella. These require a more traditional open approach to repair and reconstruct the attenuated medial retinaculum and the medial patellofemoral ligament (MPFL) tissues. These are often stretched or completely torn in a recurrently dislocated patella.
The damaged tissues are exposed adjacent to the patella, and repaired and reinforced with permanent suture to recreate the “check-reign”, or these tissues are reconstructed by transferring a tendon from another location into the path of the MPFL, attaching the new ligament into tunnels at the femur and patella.
An osteotomy is a procedure whereby the bone is cut and realigned to improve the tracking of the patella within the groove, by moving the insertion of the patella tendon into the tibial bone, by cutting the tibia and sliding the prominent tibial tuberosity medially to correct malalignment within the groove.
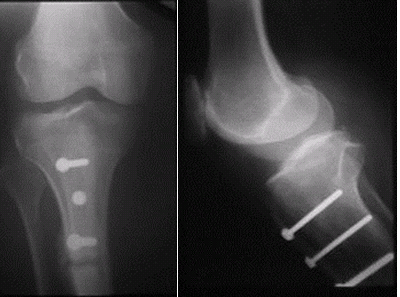
The above X-ray views show an example of a “Fulkerson osteotomy”, one type of bone realignment procedure that can be used to improve the tracking of the patella within the groove, that also reduces the loads on the patella.
Here are top-down arthroscopic views of the patellofemoral joint BEFORE (left image) and AFTER (right image) a procedure which included BOTH “proximal” and “distal” realignment techniques, i.e.- tightening the loose medial restraints above (proximal), and transferring the bone below (distal). Note normalization of alignment:
All of these procedures can be very beneficial to the patient with patella problems, but require EXTENSIVE post-operative therapy and rehabilitation to optimize outcomes. In and of themselves, they help create improved biomechanics, that COMBINED with VIGOROUS physical therapy, usually result in less symptoms. Tissue transfer and bone cutting procedures require protected weight-bearing and limitations for 4-6 weeks post-op until bone healing begins. Patella surgery, like any surgery, has risks, such as infection, stiffness, continued instability, weakness, pain, blood clots, possible need for hardware removal, fracture, impaired bone healing, etc.
Recovery ranges from 3-12 months, depending upon the type of surgery, healing rates and limitations, and patient rehabilitation and ongoing strengthening efforts.
